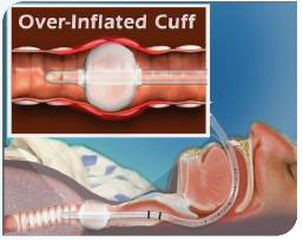
1.1 Clinic problem : cuff over-inflated
The human trachea is a very fragile tissue. As other parts of the body, its healthy functioning depends on adequate blood flow. If the pressure applied to the trachea wall is too high, blood flow to the pressured area will be reduced or completely interrupted. In this case, excessively pressured trachea tissue will appear inflammation erosion and even necrotic perforation. One of the common causes of benign tracheal stenosis is tracheal intubation, and it is the most important cause of benign tracheal stenosis, accounting for about 1/3 of all causes. At present, there are still 1% -4% of patients with tracheal intubation happen tracheal stenosis. And the main cause is improper balloon pressure management
Clinical studies have shown that granulation tissue hyperplasia and tracheal cartilage destruction collapse are two important factors for tracheal stenosis after intubation. When the tension between the balloon and the trachea wall exceeds the perfusion pressure of the tracheal mucosal capillaries (20-30mmHg), the ischemic damage to the tracheal mucosa occurs, followed by local edema and bacterial inflammation to stimulate the mucosal ulcer. When the pressure continues to increase, mechanical pressure on the cartilage ring interrupts blood flow of the perichondria, causing chondritis, and further development leads to cartilage necrosis and absorption, granulation tissue repair and or cartilage scaffold structure destruction, which eventually leads to narrowing of the trachea.
The higher the balloon pressure, the longer the time, the higher the incidence of tracheal wall injury. When the cuff pressure on the trachea wall reaches 40-80mmHg, ischemic necrosis and trachea mucosa sheds happen, and the blood flow between the trachea cartilage is interrupted cause serious complications such as trachea wall perforation and rupture; when the balloon pressure reaches 100mmHg for 15 minutes, the basement membrane begins to separate and the mucosal matrix is exposed. After 4 hours, damage and inflammation can penetrate into the cartilage.
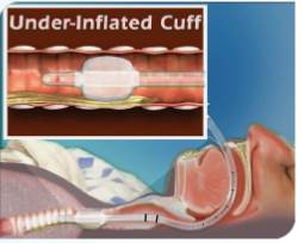
1.2 Clinical problem : insufficient inflation
Due to the slow leak of the cuff closed system, or the patient's body position change and other factors, the cuff pressure coulde be too low. If the cuff pressure is insufficient, below 20cmH2O will cause the aspiration rate to increase significantly, becoming an independent risk of VAP (ventilator-associated pneumonia, a secondary intra-pulmonary infection caused by tracheal intubation and use of the ventilator), the occurrence of VAP will generate a large amount of medical investment and even endanger the life of patients.
1.3 Clinical guidelines:
A number of VAP prevention guidelines recommend that the pressure of tracheal cuff is maintained at 25-30cmH2O in adults (China CSA Airway Management Guide); 20-30cmH2O (American ASA Anesthesia Guide); some of the latest research on pediatric artificial airway products suggest cuff pressure should be maintained at 15-20 cmH2O (the first time inflation of pediatric tracheal intubation products with Surecuff, recommended to reach 20-25cmH2O; the guideline for the laryngeal mask is 40-60cmH2O (The more lower cuff pressure, the less injury, so recommend to inflate the laryngeal mask to about 45cmH2O with Surecuff ).
2. Current clinical solutions and disadvantages:
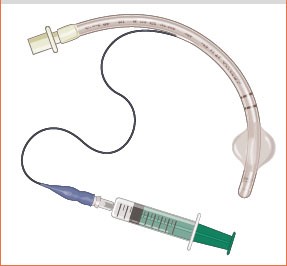
2.1 The touch judge method (TJM), also known as the finger sense method, is also the most commonly used clinical method for more than 90%.
The inflation method is to use a syringe to connect the pilot to indicate the pressure of cuff, and use finger to feel the pressure of pilot balloon. The degree of softness and rigidity of the balloon is as normal as the nose tip of a normal person.
Disadvantages: The pressure of cuff cannot be controlled accurately based on personal finger experience. Operators may tend to use higher cuff pressure, causing tracheal wall damage. And for newbies it’s difficult to judge what the right rigidity of nose tip.


2.2 Minimal occlusive volume (MOV) means that there is no gas leakage during inhalation.
Method: Place the stethoscope under the patient's thyroid cartilage to monitor for gas leaks, inject air into the cuff until no air leak is heard, then extract 0.5ml of gas, and then slowly inflate the air until the leak sound disappeared.
Disadvantages: This method is cumbersome, takes a long time, easy to cause trachea injury.

2.3 The minimum leak technique (MLT) refers to a small amount of gas leakage during inhalation.
Method: Place the stethoscope at the trachea, inflate the cuff until no air leakage is heard, and deflate 0.1ml / times until you hear a small air leakage when inhaling. This is the smallest air leakage technology.
Disadvantages are complicated operation, prone to aspiration, and affect ventilator ventilation.
2.4 quantitative inflation method:
Method: Using sizes marked syringe or by personal experience to fill different size cuff with a certain amount of air.
Disadvantage: Human trachea size is a continuous changed with N possible sizes, and because the structure of the human body varies from person to person, the product also varies from different manufacturer, so using a fixed amount of inflatable hair, the pressure of the filled cuff is either high or low.


2.5 Cuff pressure measurement (CPM) refers to the use of a dedicated pressure gauge for inflation.
Method: connect the piolet valve with pressure gauge, then extrude the airbag handle repeatedly, usually get a higher pressure than target, then pressure deflate button to deflate some air. After adjustment, the air pressure is lower than the target at high probability. So need to very gently extrude the airbag handle again to get the target pressure.
Disadvantages: Pressure gauge is a little big large, not convenient to carry in pocket. Extrude a rubber balloon in the hand, the inflation flow rate and speed are difficult to control, which causes the gauge pointer to swing too much during the inflation process, causing excessive inflation. After that, the adjustment of the deflation button must be precise and carefully. If you over-deflation, need repeat above operations again. Inject port position design some is not convient and some gauge type need a connecting tube for inflation. A lot hospital have it but don’t use it, because not convenient.
2.6 Airway products with indicators (the latest products from two manufacturers worldwide)
With a hard-shell general indication of pressure is used to replace the traditional soft finger touching balloon.




Disadvantages: 1. Low accuracy and large telerance. The target green band is very narrow (1-2mm, scale span is 10cmH2O or 20cmH2O), and around the edge of green band(still in the green band range), the pressure will be lower or higher than the ideal pressure value range. And due to the direct impact of the inflation airflow, lacks cushioning , the indicator bounces repeatedly . In addition, due to the problem of the inflation angle and the narrow green belt , it is difficult to local the indicator at the middle positon of the narrow green belt( the idea position). Usually at the edge (see the demonstration of the video by related company experiened staff); 2. Because the hard shell design, once there is a defective , because lack of a traditional touching pilot, the clinical consequences will be very serious; 3. if you don't look closely, easily misjudge the pressure of the capsule. To sum up the three defects, for the pressure requirements of the tracheal intubation of 25-30cmH2O required by the airway management guidelines, the compliance rate of this device will be very low. Also it is very difficult to inflate to the idea pressure 40-45 cmH2O for the laryngeal mask ( 40-60cmH2O by guideline).
We chat
