Clinic Problem
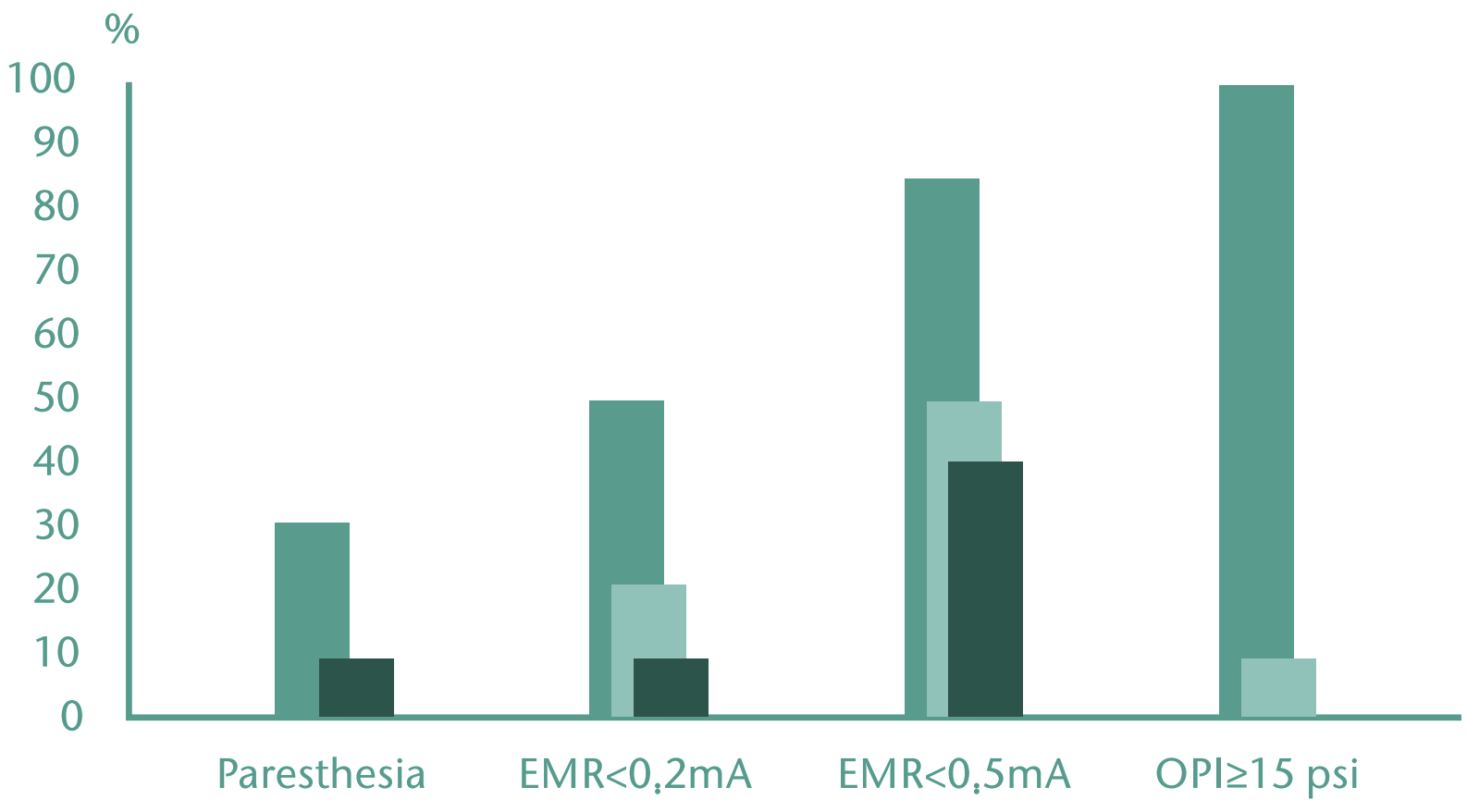
Ultrasound-guided localisation of peripheral nerves and the associated real-time visualisation provide crucial benefits in Regional Anaesthesia. However, it is clear that this does not reduce the incidence of permanent nerve damage. Even in combination with nerve stimulation, intrafascicular injections cannot be ruled out. The causes include incorrect needle position along with exceeding critical injection pressures. Research has shown that high opening injection pressure (>15psi) consistently indicates intrafascicular (chart-I) or detects needle-nerve-contact(Chart-II) injection. Therefore, avoiding injection with high opening injection pressure (>15psi) can prevent injection into poorly compliant tissue.

Nerve-contact effects:
Direct needle-nerve contact can lead to damage of the neural structures with subsequent transient or permanent neurological impairment. Localization control using ultrasound and/or nerve stimulation may not in all cases reliably indicate direct needle-nerve contact. Paresthesia in and of itself is not regularly observed. Avoiding direct needle-nerve contact minimizes the risk of damage to the nerve wall.
Fascia-contact effects:
Injections administered in the wrong tissue layers can cause anesthesia failures. A high opening pressure may indicate occlusion of the tip of the needle due to the fascia in front of it.
Intrafascicular effects:
In the case of intrafascicular injection at high pressure lasting several hours, the microvascular blood supply of the nerve is severely restricted, which can lead to degeneration of nerve structures.
Chart-I
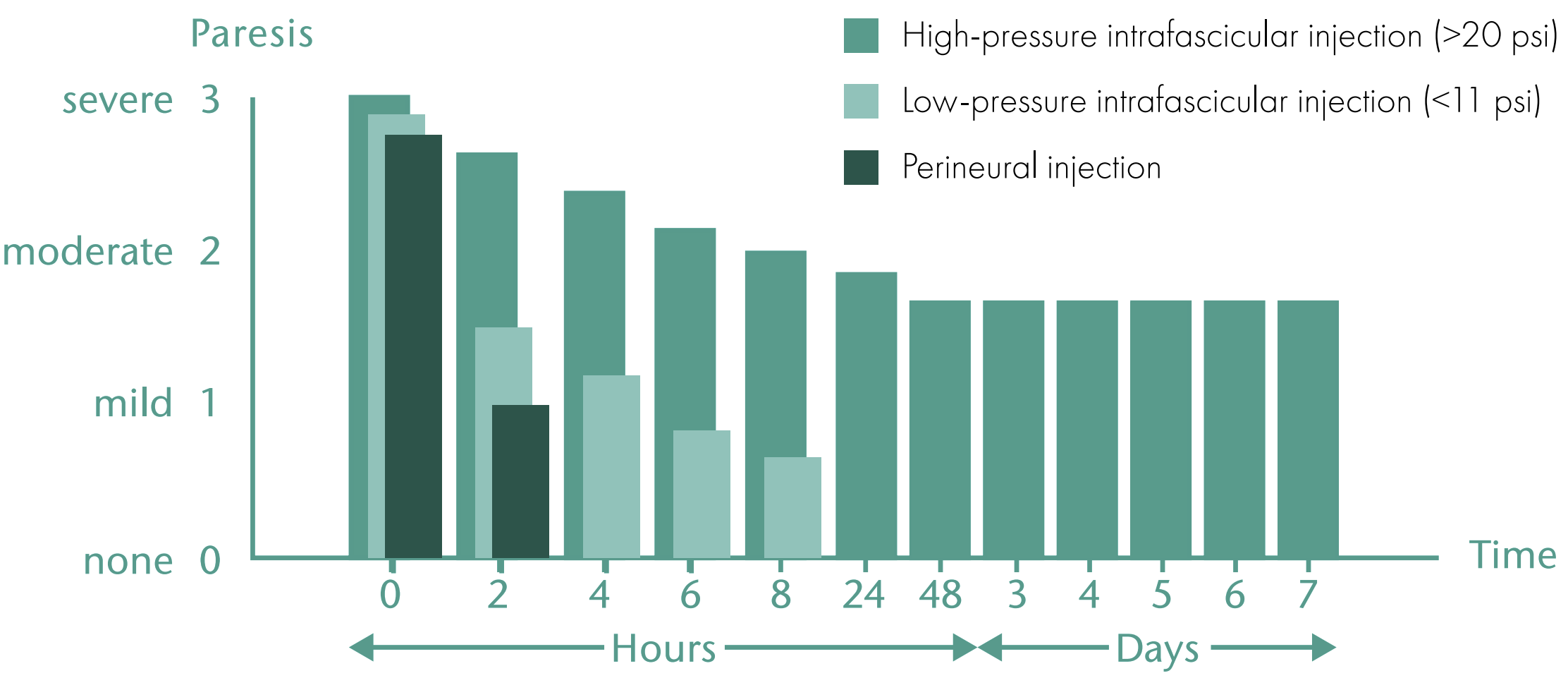
Chart-II

We chat
